Revenue Cycle Management (RCM)
RCM Software
Faster, Error-Free Billing
Clinicmaster’s revenue cycle management software helps healthcare providers simplify billing, reduce claim denials, and accelerate reimbursements. Our RCM solution ensures a smooth flow of revenue, from automated claims processing, intelligent payment tracking and real-time financial analytics, so that your team can focus on patient care instead of chasing payments.
Book a Demo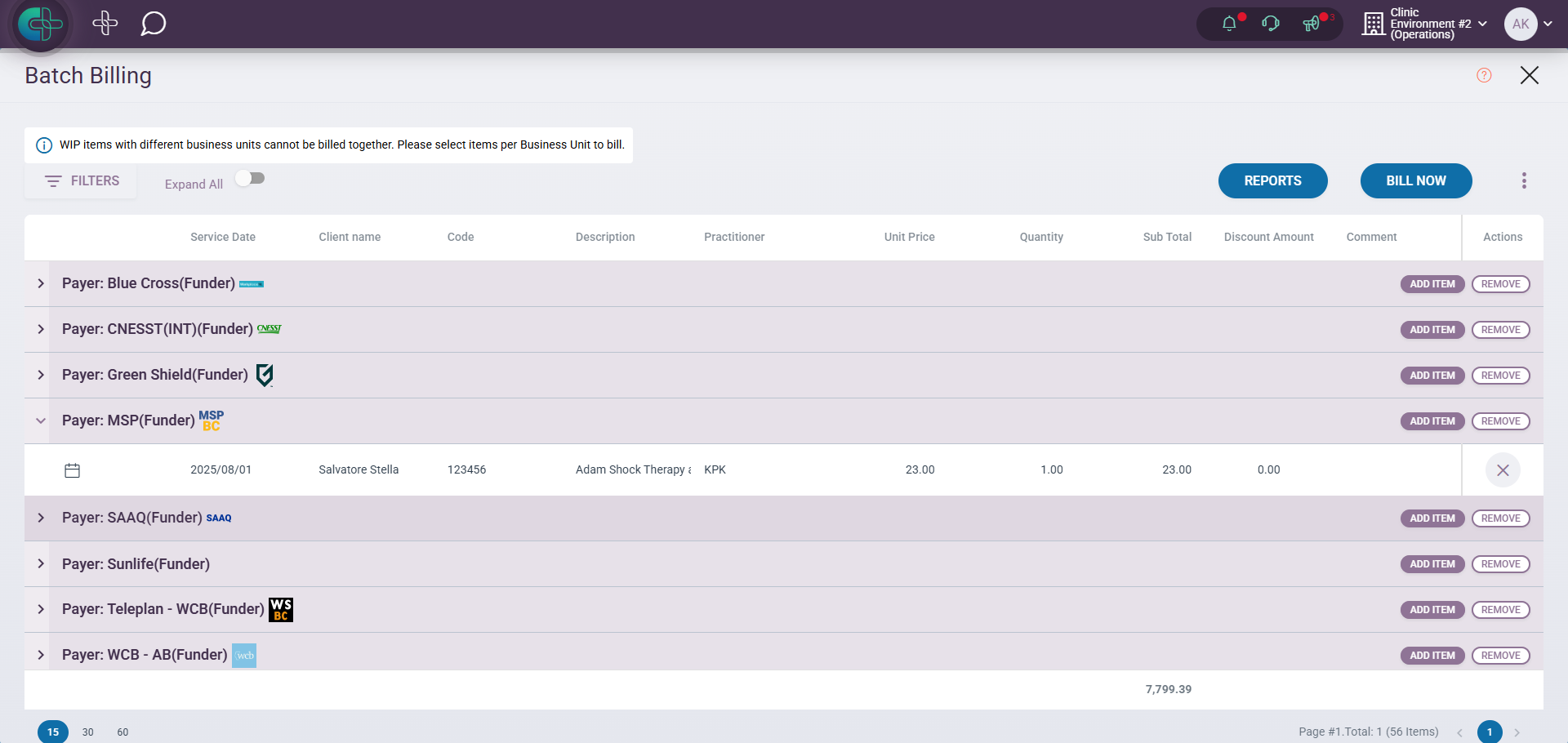

Core Features of Our Revenue Cycle Management Software
Automated Claims Processing
Submission, tracking, and payment posting in one workflow
Real-Time Eligibility Verification
Prevent denials before service delivery
Intelligent Payment Tracking
Match payments to claims automatically

Financial Dashboards and Analytics
Monitor performance and trends at a glance
Integration with EMR and Scheduling
Connect care, scheduling, and billing seamlessly

Secure, Compliant Payment Processing
Built to meet HIPAA and PIPEDA requirements
How Our RCM Software Works
Traditional billing processes are manual, error-prone, and slow. Clinicmaster changes this by providing an integrated platform that connects your clinical, scheduling, and billing workflows. Designed for private practices, group clinics, and multi-location organizations, our RCM software automates the entire revenue cycle while maintaining compliance.
Streamlined Claims Submission and Processing
Automated claim creation, eligibility verification, and intelligent scrubbing ensure accurate submissions the first time.
Faster Reimbursements with Fewer Errors
Real-time claim validation reduces denials and shortens turnaround time for reimbursements.
Centralized Billing Across Multiple Providers or Locations
One system to manage billing for individual providers, departments, or multi-site clinics—ensuring consistency and oversight.

Clinicmaster By The Numbers
0
(Up to) First-Pass Claim Acceptance Rate
0
Faster Reimbursement Cycle Times
0
Reduction in Billing Errors
0
Compliance with Canadian & U.S. Regulations
0
Time Savings for Multi-Location Billing Teams
Problems We Solve
Challenge
Our Solution
Delayed reimbursements
Automated claims and payment posting
High rate of billing errors
Real-time validation and error flagging
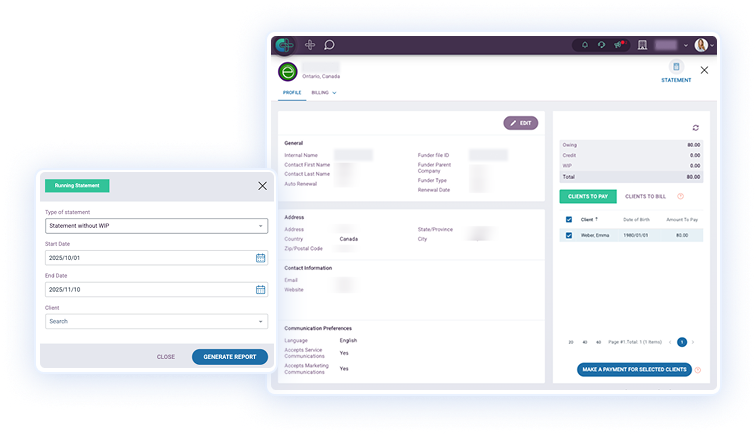
Poor visibility into receivables
Financial dashboards and reporting tools
Manual, time-consuming billing
Integrated, automated workflows
Simplify Your Entire Billing Workflow
Claims are generated automatically from clinical encounters, reducing manual entry and preventing costly errors. We ensure claims are accurate before submission with built-in validation checks, leading to fewer rejections and faster reimbursements.
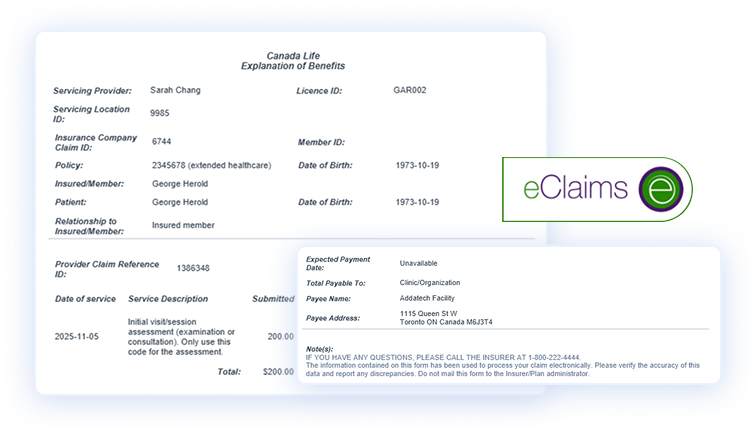
Payments are matched directly to claims in real time, making reconciliation effortless. Patient accounts are instantly updated via automated posting, which also flags exceptions for review, thereby eliminating hours of manual tracking.
Customizable dashboards provide clear visibility into collections, denial trends, and outstanding claims. With real-time reporting, you can make data-driven financial decisions and identify areas to improve cash flow.
Key Use Cases
I want to reduce claim denials and speed up reimbursements.
We need a unified billing and payment system for our entire clinic.
I want to track revenue performance in real time without spreadsheets.
Who Our RCM Software is For
- Private practices and group clinics
- Billing teams handling high claim volumes
- Canadian healthcare providers seeking compliant billing software in Canada
- Multi-location practices needing centralized revenue tracking
Canadian Billing Compliance and Integration
Clinicmaster’s billing software is designed for compliance with provincial and federal regulations within Canada.
- Supports OHIP, MSP, Teleplan, CNESST, HCAI, Telus e-claims, Pacific Blue Cross, Greenshield
- Compliant with SOC 2, HIPAA, and PIPEDA standards
- Flexible for multi-payer environments and insurance workflows
Frequently Asked Questions
Yes, Clinicmaster supports provincial systems and private insurance workflows.
Yes. Claims can be submitted and tracked across multiple payers simultaneously.
We reduce claim denials with real-time validation and an AI reconciliation tool for select payers.
Yes. Our centralized dashboard consolidates billing data across your entire organization.
Yes. Clinicmaster meets HIPAA and PIPEDA standards with secure, encrypted transactions.


